By: Jeremy Howard, Distinguished Data Scientist, University of San Francisco, and Vincent Rajkumar, Editor in Chief, Blood Cancer Journal
Today, it is widely accepted by the public health and scientific community that two of the most effective tools we have to stop the spread of COVID-19 are distancing and masks. Everyone is asked to keep at least six feet apart, since it’s generally believed that most airborne droplets fall to the ground inside that distance. They are also asked to wear a mask, to stop the droplets from being ejected in the first place, and also to reduce the radius of the “germ cloud” caused by the droplets. Since around half of transmission occurs from people that don’t know they’re sick, people are asked to follow these guidelines even if they don’t have symptoms.
Unfortunately, Dr. Michael Osterholm and the Center for Infectious Disease Research and Policy at the University of Minnesota (CIDRAP) which he leads have been pushing misleading information about masks since early in the pandemic.
Dr. Michael Osterholm is head of CIDRAP, and is one of our country’s top experts on infectious diseases. He has been a strong advocate for the importance of physical distancing. But when it comes to the efficiency of cloth masks, the only realistic type of mask available to most of the public, Osterholm and his CIDRAP colleagues are using their platform to promote misinformation to the public.
WCCO radio announced that “Coronavirus expert Dr. Osterholm questions guidelines on cloth masks, says they don’t stand up to virus’ air assault”, quoting Osterholm as saying “Cloth masks, I think… have little impact, if any.” In another WCCO appearance he stated that “the Minneapolis mask mandate could do more harm than good”. The Cape Charles Mirror stated “You realize, the stupid masks you wear to the store don’t do anything, right”, quoting Osterholm: “If you want to wear a cloth mask, use it. Know that I don’t believe, or none of my colleagues, that this is going to have a major positive impact.”
In April CIDRAP published a piece from Lisa Brosseau, an industrial hygienist, and Margaret Sietsema, a public health academic, which is full of uncited claims, falsehoods, and misunderstandings. Unfortunately, the article was not submitted for peer review, nor was any mechanism for public comment made available, despite Osterholm’s stating a concern about studies that are “being widely distributed before they are reviewed and published”. It claimed, without any references, that “sweeping mask recommendations… will not reduce SARS-CoV-2 transmission, as evidenced by the widespread practice of wearing such masks in Hubei province”. No references or data were provided to back up this claim.
Looking at the actual data, however, shows that it supports the opposite conclusion – masks may have been critical in controlling the Hubei outbreak. A report from Guo Yi in HK01 pointed out that up until Jan 22 most people in Wuhan were not wearing a mask. The next day, the government started requiring masks in public. Wuhan had their peak number of cases two weeks later, on Feb 4, and since then case numbers have been decreasing. Two weeks is exactly the amount of time we’d expect to see a public health intervention like this take to impact documented cases.
The article cites 4 references for a claim that “Household studies find very limited effectiveness of surgical masks at reducing respiratory illness in other household members”. However, none of the references make this claim or show data to support it. Their reference 22, for instance, is a meta-analysis which lists the results of each analysis they looked at, and concludes “If the randomized control trial and cohort study were pooled with the case–control studies, heterogeneity decreased and a significant protective effect was found”.
The article further claims, with no references, that “Our review of relevant studies indicates that cloth masks will be ineffective at preventing SARS-CoV-2 transmission, whether worn as source control or as PPE”. However, it presents no studies that provide evidence that cloth masks will be ineffective at preventing SARS-CoV-2 transmission.
Brosseau and Sistema claim that there was a “failure of cloth masks required for the public in stopping the 1918 influenza pandemic”, citing a 1920 paper by WH Kellogg, a claim repeated in a polemic from Osterholm in a recent podcast. This is a misunderstanding of the evidence. In fact, Kellogg relied on looking at the difference in results between San Francisco, where masks were required, and other regions where they were not. Using a single data point in this way is an example of the ecological fallacy, and is not considered in modern epidemiology as meaningful evidence. However, even if we do accept that the San Francisco mandate was ineffective, we should also note what Kellogg said about why: his belief was that the problem was that masks were only used outside, where transmission was less likely. In Australia, mask-wearing by healthcare workers was thought to be protective during the 1918 pandemic, and given evidence of transmission in a closed railway carriage, it was concluded that mask wearing “in closed tramcars, railway carriages, lifts, shops, and other in enclosed places frequented by the public had much to recommend it.” Today, nearly all places that require masks for COVID-19 only require them inside.
There was also a problem with the fine gauze material recommended for masks in the 1918 pandemic. Dr Wu Lien-teh, the first Chinese to graduate in medicine from Cambridge, popularized the use of the mask globally, thanks to his research showing its efficacy for slowing the transmission of the 1910 Manchurian Plague. He explained that an absorbent inner layer of cotton wool was needed. The prominent French physician Gérald Mesny, however, was not convinced that such a mask could be of any use. As Wu narrates in his auto-biography, Plague Fighter:
The Frenchman was excited, and kept on walking to and fro in the heated room. Suddenly, unable to contain himself any longer, he faced Dr. Wu, raised both his arms in a threatening manner, and with bulging eyes cried out ‘You, you Chinaman, how dare you laugh at me and contradict your superior?’
Mesny spent the next few days walking amongst Manchurian Plague patients without wearing a mask. Predictably, he died of the disease shortly thereafter.
Unfortunately, Wu’s construction advice was forgotten or ignored by the time of the 1918 flu pandemic. During that time, most people were using very loose fabric, like cheesecloth.
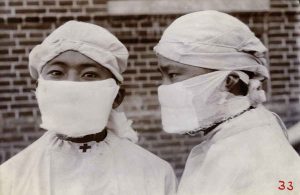
Early photos of pneumonic plague epidemics; from Manchurian Plague Prevention Service
Mind you, we should be careful not to assume that findings from the 1918 flu should be applied directly to COVID-19. If we do, we might just give up on every public health intervention. The World Health Organization states that based on the 1918 flu:
- “social-distancing measures did not stop or appear to dramatically reduce transmission”
- “closing schools, churches, and theaters was not demonstrably effective in urban areas”
- “more influenza cases developed among pupils in a Chicago school after a holiday than when schools were in session”
- “complete quarantines” were “lamentably inefficient in checking the spread of the disease”
Osterholm said in his podcast, “I hope if nothing else “so-called” experts on the various issues related to COVID-19 learn to stay in their professional lanes”. In particular, he said that “the vast majority of information you’re hearing every day in the popular literature or even in the news about cloth masks is not coming from anyone with any expertise in aerosol science”. However, no aerosol scientists are listed on CIDRAP’s staff page, or were involved in the Brosseau paper. On the other hand, a letter he derides as from “so-called experts” includes three noted aerosol scientists as signatories, and the paper it draws from has one of the world’s top aerosol scientists as a co-author.
In the podcast, Osterholm claims that “in the earliest days of this pandemic we knew that breathing air would be the main way the virus would be transmitted”. We knew no such thing then, and we don’t know it now. In fact, we now know that COVID-19 results in viral shedding in the upper respiratory tract, where speech can result in significant droplet formation. The CDC states that “the virus is thought to spread mainly from person-to-person, between people who are in close contact with one another (within about 6 feet), through respiratory droplets produced when an infected person coughs, sneezes, or talks.” Few if any pre-symptomatic or asymptomatic patients show significant lower respiratory tract shedding, which would be required for breathing to be a transmission vector.
This is not the first time that Osterholm has jumped to early conclusions, well in advance of evidence. Early in the pandemic, CNN warned that China says coronavirus can spread before symptoms show. Osterholm dismissed it. “I seriously doubt that the Chinese public officials have any data supporting this statement,” he said, “I know of no evidence in 17 years of working with coronaviruses — SARS and MERS — where anyone has been found to be infectious during their incubation period.”
Osterholm goes on to quote from the US Surgeon General, who said on Twitter that masks “are NOT effective in preventing general public from catching #Coronavirus.” Anthony Fauci has since then explained that the reason for this policy in the early days of the pandemic was due to concerns about a lack of supply for health-care workers, rather than a genuine view that masks were not useful. The Surgeon General has since that time walked back those claims and now heavily promotes community mask wearing.
Osterholm then discusses a Cochrane review, which concluded that “Surgical masks or N95 respirators were the most consistent and comprehensive supportive measures. N95 respirators were non‐inferior to simple surgical masks but more expensive, uncomfortable and irritating to skin.” Osterholm claimed that “their review results did not provide strong evidence.” The reason that a Cochrane review can never provide strong evidence is that they are designed for clinical studies, not broad public health measures, and both the WHO and Cochrane guidelines make clear that different types of evidence need to be looked at in these cases. Specifically, it’s not generally possible to complete a randomized controlled trial (RCT) of a broad public health measure with population level impacts, due to unavoidable ethical and logistical obstacles.
The closest thing we have, perhaps, to a relevant RCT is the paper The First Randomized, Controlled Clinical Trial of Mask Use in Households to Prevent Respiratory Virus Transmission: This was an Australian study for influenza control in the community, but not during a pandemic, and without any enforcement of compliance (such as would be provided by a mask mandate). It stated that “observational epidemiologic data suggest that transmission of viral respiratory infection was significantly reduced during the SARS epidemic with the use of face masks as well as other infection control measures” and “in an adjusted analysis of compliant subjects, masks as a group had protective efficacy in excess of 80% against clinical influenza-like illness.” However, the authors noted that “we found compliance to be low, but compliance is affected by perception of risk. In a pandemic, we would expect compliance to improve. In compliant users, masks were highly efficacious.”
Trisha Greenhalgh, an Oxford professor and author of Applications of Evidence Based Healthcare, noted the importance of drawing on a “wider evidence base” than just RCTs in studying mask use. She finds that the “various streams of evidence contribute, in different ways and at different levels, to strengthen the argument for recommending face coverings, especially in crowded public places where social distancing is impossible, during the pandemic.” In another paper, Greenhalgh et al warn that systematic reviews (such as Cochrane reviews), which can only “address narrowly focused questions”, should be used with care, otherwise “the absence of thoughtful, interpretive critical reflection can render such products hollow, misleading and potentially harmful”.
Osterholm also quotes from a report from the Usher Network for COVID-19 Evidence Reviews (UNCOVER), but failed to quote from the relevant section, which actually concluded that “homemade masks worn by sick people can reduce virus transmission by mitigating aerosol dispersal. Homemade masks worn by sick people can also reduce transmission through droplets. By reducing the number of droplets reaching surfaces, homemade masks can reduce the risk of transmitting or acquiring COVID19 through reducing environmental (surface) contamination”.
The next part of the podcast discusses a paper from De Kai et al describing the results of two epidemiological models. Part of Osterholm’s criticism is based on the backgrounds of the authors, rather than the content of the paper. The other part is based on a misunderstanding of a model in the paper, which appears to stem from Osterholm’s lack of background in modeling. He describes the paper as an SEIR model; however the paper actually shows the results of two models, one of which is an agent based model (ABM). A compartmentalized SEIR model is used to cross-check the ABM. A critical part of the basis of an ABM is that it has a concept of time, which Osterholm incorrectly states it does not account for. Further, the parameters of the model allow for time and dose relationships to be varied.
Osterholm makes a surprising claim that “the results of this modeling study has been the basis for people making major policy decisions”. In fact, there have been numerous modeling studies, all of which have shown the same results, using a variety of different approaches. There is no single study that has been the basis for people making decisions.
He then covers a letter to US governors that I co-wrote, which was signed by over 100 scientists from around the world. In response, he correctly states that “The cloth that serves as the filtration for the mask is meant to trap particles being breathed in and out. But it also serves as a barrier to air movement because it forces the air to take the path of least resistance, resulting in it going in and out at the sides of the mask.” However, he appears not to be aware that this issue has been well studied and measured by aerosol scientists and fluid dynamics experts. In particular, Schlieren imaging shows that during normal breathing nothing escapes around the sides of a cloth mask. Even during coughing, a cloth mask dramatically decreases the radius of the droplet cloud and the number of droplets it contains. There is still a lot we don’t know about the relative impact on transmission of the different particle sizes released during breathing and speaking, and about exactly how much of each size different types of mask can filter, but we do know that cloth masks block many particles effectively.
He goes on to cast doubt on the validity of population level analysis, saying “in countries experiencing COVID-19 outbreaks many other control measures were put in place at the same time that mask use may have increased”. Whilst this is true, models can try to account for these by including other measures as confounding variables. Multivariate analyses have been completed that do just that, and still show strong results from mask use. Osterholm argues that “There is simply no credible data to support the claim” that “laws appear to be highly effective in increasing compliance in slowing or stopping the spread of COVID-19.” However, the multivariate analysis from Leffler et al specifically uses mask laws as an independent variable, showing exactly the data that Osterholm claims does not exist.
Finally, Osterholm refers to a study by Raina Macintyre et al “that was carried out in healthcare workers, not the general public. In short, the study found that those that wore the cloth masks had 13 times more infection outcomes than those that wore surgical masks.” This is a misunderstanding of the study and its results. The study found that a supply of just five cloth masks for a four-week period was not effective as PPE for rhinovirus, compared to a regular supply of two new surgical masks every day. This is consistent with a more recent study that found that simple masks were not effective for blocking rhinovirus; however, that study found them 100% effective at blocking seasonal coronavirus. Osterholm failed to note, however, that since that time Raina Macintyre has also published a study on the use of cloth masks for COVID-19, finding that “face mask use by the primary case and family contacts before the primary case developed symptoms was 79% effective in reducing transmission”.
Osterholm has already recognized and highlighted the importance of distancing, despite a lack of randomized controlled trial evidence. And yet if all that mattered really was the aerosol particles that Osterholm is so focused on, distancing would be of little value, since those particles can remain in the air for hours and can wander all around a building. In practice, however, we see that nearly all spreading occurs within a couple of meters of a patient (except in cases such as singing and yelling, where droplets are ejected much further), and the droplets hang around for about 10 minutes. The same observations about real world cases that support the importance of distancing also support the importance of mask use. In fact, the two interventions make an excellent pairing: mask use decreases the radius of the droplet cloud, making distancing more effective.
Today, the CIDRAP web site still makes the claim that “sweeping mask recommendations… will not reduce SARS-CoV-2 transmission”. Correcting the record at this point will require an unambiguous, public statement, that these earlier claims were not based on scientific evidence, that they were wrong, and that mask use is a very important tool to combat the spread of COVID-19.